Rosacea is a chronic facial skin condition of unknown cause. Similar to Psoriasis.
Rosacea is a common inflammatory skin disorder that can seriously impair quality of life.
According to Louisiana State University and American Family Physician — It is characterized by marked involvement of the central face with transient or persistent erythema, telangiectasia, inflammatory papules, and pustules, or hyperplasia of the connective tissue.
Transient erythema, or flushing, is often accompanied by a feeling of warmth.
It usually lasts for less than five minutes and may spread to the neck and chest.
Less common findings include erythematous plaques, scaling, edema, phymatous changes (thickening of the skin due to hyperplasia of sebaceous glands), and ocular symptoms.
The National Rosacea Society Expert Committee defines four subtypes of rosacea (erythematotelangiectatic, papulopustular, phymatous, and ocular) and one variant (granulomatous).
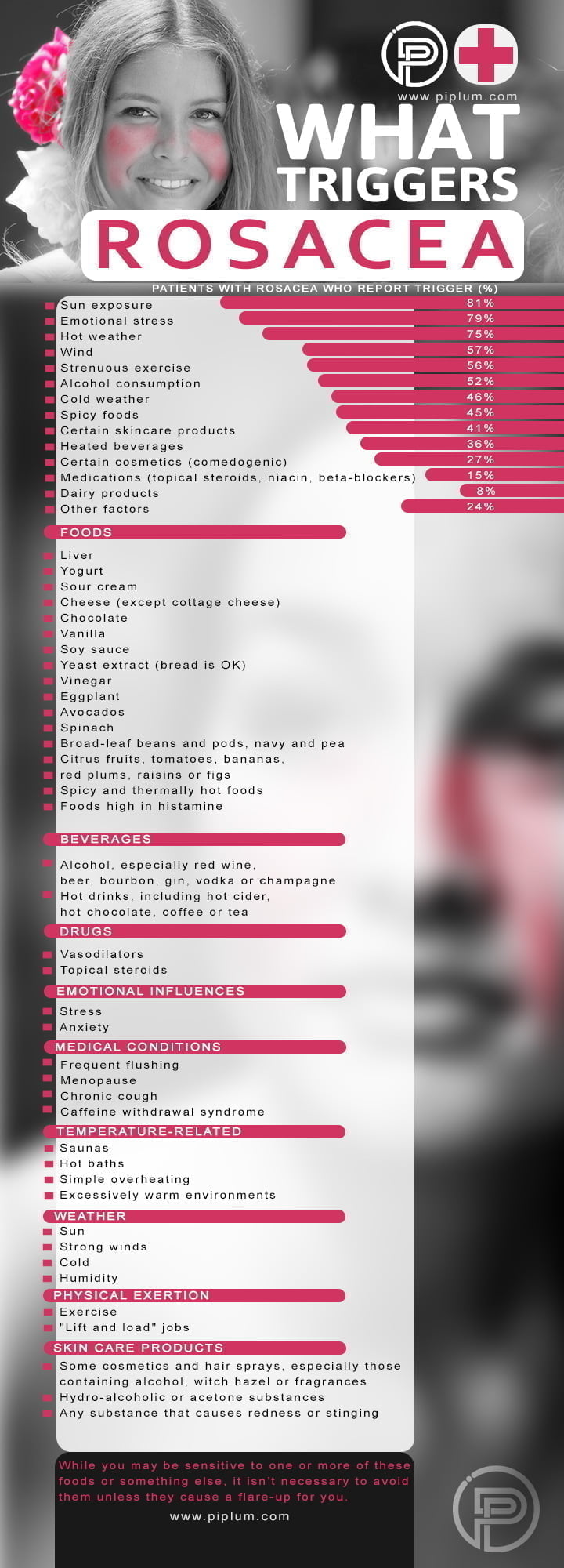
Treatment starts with avoidance of triggers and the use of mild cleansing agents and moisturizing regimens, as well as photoprotection with wide-brimmed hats and broad-spectrum sunscreens (minimum sun protection factor of 30).
For inflammatory lesions and erythema, the recommended initial treatments are topical metronidazole or azelaic acid.
Once-daily brimonidine, a topical alpha-adrenergic receptor agonist, is effective in reducing erythema.
Papulopustular rosacea can be treated with systemic therapy including tetracyclines, most commonly subantimicrobial-dose doxycycline.
Phymatous rosacea is treated primarily with laser or light-based therapies.
You might like: Health Benefits Of Dandelion Flower: Heals The Skin, Helps To Lose Weight, Protects Against Cancer
Ocular rosacea is managed with lid hygiene, topical cyclosporine, and topical or systemic antibiotics.
How To Treat Rosacea And How To Detect Symptoms?
Rosacea is a common inflammatory skin disorder that can seriously impair quality of life.
Treatment starts with general measures which include gentle skin cleansing, photoprotection and avoidance of exacerbating factors such as changes in temperature, ultraviolet light, stress, alcohol and some foods.
To fight rosacea — avoid triggers and carry your skin. While you may be sensitive to one or more things on this list, it isn’t necessary to avoid them.
Rosacea Symptoms And Triggers. Manage Your Skin Health. Poster.
Symptoms and Treatment of Rosacea
Understanding how to treat rosacea is, of course, the number one question people ask once their symptoms are diagnosed. (According to: rosacea-skin-care.com)
You might like this article: Discover Magical Properties of Flaxseed Oil. What Features Does It Have?
The answer, however, depends on a few things, including what symptoms you are presenting with, what triggers those symptoms and what your preferred philosophy is on health care.
Although there is no cure for rosacea, it is most certainly manageable.
You might like: Gestational Diabetes? The Best Way To Deal With Pregnancy Risks.
By “manageable” we mean that with the right approach (for you), you can eliminate the symptoms.
Because rosacea can present a variety of symptoms, scientists classified it into four subtypes that correspond to the most common groupings of symptoms.
Subtypes of Rosacea:
- Subtype 1 (erythematotelangiectatic) This is what people think of when they hear rosacea. This represents the redness, visible broken veins, and flushing.
- Subtype 2 (papulopustular) This takes all the same issues from Subtype 1 and adds in fluid-filled pimple and itchy bumps.
- Subtype 3 (Rhinophyma/Phymatous) Causes a thickening of the skin, usually on the nose. The most famous example is W.C Fields.
- Subtype 4 (ocular rosacea) This is characterised by red and sore eyes that often feel gritty.
Subtypes of rosacea
Treatment and drugs of Rosacea
Treatment can be optimized according to the dominant features.
Topical therapies are recommended for at least six weeks to effectively review the response. Topical corticosteroids should be avoided.
Treatment for flushing and erythema may involve oral drugs with vasoconstriction properties including adrenergic antagonists including mirtazapine (alpha-blocker), propranolol (beta-blocker) or carvedilol (both alpha and beta-blocker).
You might like this article: Food For a Healthy Gut. Discover Purple and Blue Fruits and Vegetables.
These are used at low doses to avoid adverse effects such as hypotension, somnolence, fatigue, and bronchospasm.
They should be prescribed under specialist supervision, and careful monitoring is required.
Clonidine is an oral alpha2 agonist that has been used for flushing.
You like this article: Save Your Skin From this Dangerous Disease. How to Detect Skin Cancer.
However, topical alpha2 agonists are preferred because they target the skin and carry less risk of systemic adverse effects.
Brimonidine is a topical alpha2 agonist that can reduce erythema for up to 12 hours through direct cutaneous vasoconstriction.
Brimonidine 0.33% gel is very useful for some people when not used daily.
Post-treatment rebound erythema may occur, and in general, telangiectases will not clear.
Treating Erythematotelangiectatic Rosacea
Topical treatments for this form of rosacea include metronidazole, azelaic acid, and brimonidine. They can be used alone or in combination.
Metronidazole works as an anti-inflammatory drug by altering neutrophil chemotaxis and inactivating reactive oxygen species.
Metronidazole 0.75% has been shown to reduce erythema, papules and pustules in multiple trials of patients with moderate to severe rosacea.
Related: Pamper Yourself: Homemade Beauty Treatments. Cheap Face Masks.
It is usually well tolerated with minor local adverse effects such as skin irritation.
Topical azelaic acid is an over-the-counter preparation that has anti-inflammatory, anti-keratinizing and antibacterial effects.
A 15% gel and 20% lotion are available and can be applied once or twice daily.
Adverse effects may include skin irritation, but azelaic acid is usually well-tolerated and can be used for long periods.
Laser therapy, including vascular lasers or intense pulse light, may help to reduce refractory background erythema and clinically significant telangiectases, but will not reduce the frequency of flushing episodes.
Different laser therapies that target the vessels have been used such as 595 nm pulsed dye laser, Nd: YAG and other vascular lasers, or intense pulsed light therapy.
These should be administered by an experienced and trained laser therapist and the number of sessions and length of treatment varies for each individual.
Treating Papulopustular Rosacea
Combining topical treatments with oral antibiotics may be needed for papulopustular rosacea. Topical treatments include metronidazole, azelaic acid, ivermectin, and dapsone.
Ivermectin (1% cream) is useful for mild to moderate rosacea.
It has an anti-inflammatory effect as well as affecting Demodex mites, which may activate the local immune response to produce the pustules.
It is applied once daily for up to four months, and the course may be repeated if needed.
Topical dapsone is a sulfone antibacterial with anti-inflammatory actions. It was recently approved for acne in Australia, but in the USA it is approved for rosacea.
Dapsone 7.5% gel is applied once daily for up to 12 weeks. It should be avoided in those with known glucose-6-phosphate dehydrogenase deficiency.
Oral antibiotics used in papulopustular rosacea include minocycline, doxycycline, erythromycin, clarithromycin, and clindamycin.
Their effectiveness at sub-antimicrobial doses is mostly due to their anti-inflammatory properties rather than a direct antimicrobial mechanism. Although bacteria may contribute to this form of rosacea, evidence for this is scant.
Doxycycline 40 mg per day is commonly given in the USA as a sub-antimicrobial dose. The risk of resistance at this dose is less than with higher doses.
In Australia, 50 mg daily is used (range 25–100 mg). Photosensitivity is the main adverse effect, and sun avoidance or sunscreens may be required, especially during the summer months.
Minocycline is probably a more effective agent but the increased risk of pigmentation, liver disorders, and lupus-like syndrome limits its long-term use.
The goal of oral therapy is to improve the rosacea to a point where control is achieved by topical therapies.
Treatment duration varies from four weeks to suppress flares to many months for long-term disease suppression.
With lower doses, adverse effects like headache, photosensitivity, diarrhea and mucosal candidiasis are relatively uncommon. The antibiotics should be taken with food.
Erythromycin and clarithromycin are generally used in patients who are intolerant or have the refractory disease to tetracyclines (e.g. doxycycline, minocycline).
Topical or oral erythromycin is sometimes used in pregnant women with papulopustular rosacea.
Oral isotretinoin is usually reserved for patients who are intolerant to oral or systemic therapies.
Its effect is thought to be secondary to the downregulation of the local cutaneous immunity, although an alteration in the lipid environment of the skin cannot be excluded. Low-dose isotretinoin (10 mg daily) may be effective and have fewer adverse effects.
The teratogenicity and adverse effects of isotretinoin require routine clinical and laboratory monitoring for safety.
Referral to a dermatologist is therefore recommended!
And one more thing…
As famous inspirational quote by Stephen Hawking says:
As I don’t have much positive to say about motor neuron disease, but it taught me not to pity myself because others were worse off, and to get on with what I still could do. I’m happier now than before I developed the condition.